The field of wound care has witnessed a revolutionary advancement with the development of intelligent drug delivery systems for wound dressings. These cutting-edge technologies are transforming how chronic and acute wounds are treated, offering targeted therapy with minimal human intervention. By integrating responsive materials, sensors, and controlled-release mechanisms, smart dressings promise to accelerate healing while reducing complications.
Traditional wound dressings have long served as passive barriers, protecting injuries from external contaminants while maintaining a moist environment. However, they lack the ability to actively participate in the healing process or respond to changing wound conditions. The emergence of smart dressings addresses these limitations by incorporating advanced functionalities that monitor wound status and deliver therapeutics precisely when and where they're needed.
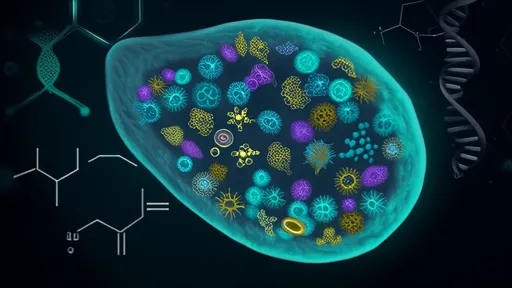
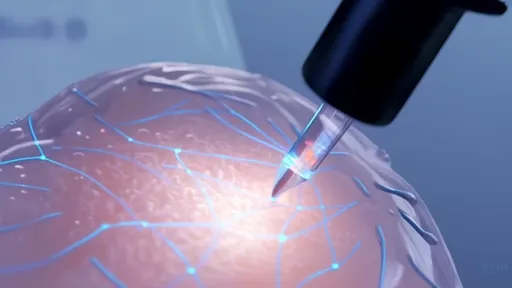
The core innovation lies in the dressing's ability to detect biochemical markers associated with wound healing phases. pH levels, temperature fluctuations, enzyme concentrations, and inflammatory biomarkers can all trigger the release of appropriate medications. For instance, when a dressing senses elevated protease levels indicating excessive inflammation, it might release anti-inflammatory drugs to rebalance the wound environment.
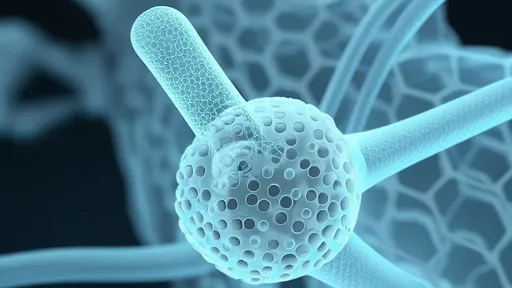
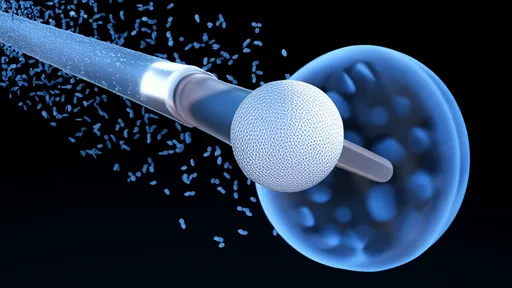
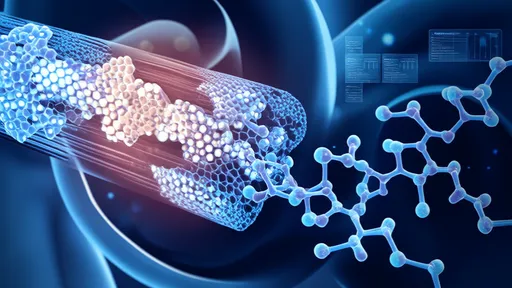
Materials science plays a pivotal role in these intelligent systems. Researchers have engineered various stimulus-responsive polymers that change their structure when exposed to specific wound conditions. Temperature-sensitive hydrogels can expand or contract to modulate drug release, while pH-sensitive nanoparticles dissolve at predetermined acidity levels to expose their therapeutic payload. Some dressings even incorporate conductive polymers that can transmit electrical signals based on wound moisture content.
Antibiotic delivery represents one of the most crucial applications for smart wound dressings. Chronic wounds often suffer from bacterial biofilms that resist conventional antibiotics. Smart systems can detect bacterial presence through chemical signals or temperature changes, then release precise doses of antimicrobial agents directly into the biofilm. This targeted approach minimizes systemic side effects while overcoming antibiotic resistance mechanisms.
The integration of biosensors takes these dressings beyond simple drug delivery. Miniaturized sensors embedded in the dressing material can continuously monitor multiple wound parameters, transmitting data wirelessly to healthcare providers. This real-time monitoring enables timely clinical interventions before complications arise. Some experimental models even incorporate machine learning algorithms that predict healing trajectories based on accumulated sensor data.
Chronic wound management stands to benefit enormously from these technologies. Diabetic foot ulcers, venous leg ulcers, and pressure sores that resist conventional treatment often require frequent dressing changes and clinical monitoring. Smart dressings could extend the time between changes while providing continuous therapy, significantly improving patient comfort and reducing healthcare costs. Early clinical trials have shown particular promise in diabetic wound care, where precise control of the wound environment is critical.
Manufacturing these sophisticated systems presents unique challenges. The dressing must remain flexible and comfortable while housing complex drug delivery mechanisms. Researchers are exploring various fabrication techniques, from 3D printing of layered materials to electrospinning of nanofiber matrices that encapsulate therapeutic compounds. Scalability and cost-effectiveness remain hurdles for widespread clinical adoption.
Regulatory pathways for smart wound dressings are evolving alongside the technology. Agencies like the FDA are developing new frameworks to evaluate these combination products that straddle the line between medical devices and drug delivery systems. The approval process must assess both the physical dressing components and the pharmacological aspects of the released medications, creating complex requirements for manufacturers.
Looking ahead, the next generation of smart dressings may incorporate even more advanced features. Experimental prototypes are exploring the use of stem cells, growth factors, and even gene therapy delivered through dressing materials. Some researchers are working on self-powered systems that harvest energy from wound exudate or body movement to operate their sensing and delivery components. The ultimate goal remains creating autonomous wound care systems that can adapt therapy in real-time without clinician input.
The economic implications of widespread smart dressing adoption could be substantial. While individual smart dressings carry higher upfront costs than conventional products, their potential to reduce healing times, prevent complications, and decrease hospital readmissions may lead to significant overall savings. Health systems worldwide are closely monitoring outcomes data to determine the true value proposition of these innovative technologies.
Patient experience represents another critical dimension of smart dressing development. Traditional wound care often involves painful dressing changes and frequent clinical visits. Smart systems designed for extended wear could minimize these traumatic interventions while providing more consistent therapeutic benefits. User-friendly designs that allow for normal mobility and water resistance are becoming priorities for product developers.
As research progresses, interdisciplinary collaboration continues to drive innovation in this field. Material scientists work alongside pharmacologists, electrical engineers partner with clinicians, and data analysts team up with product designers to overcome technical challenges. This convergence of expertise accelerates the translation of laboratory discoveries into clinically viable products that could redefine standards of wound care.
The transition from research prototypes to commercially available products is already underway. Several smart dressing technologies have received regulatory approval in various markets, with more in advanced clinical trials. As manufacturing processes mature and clinical evidence accumulates, these intelligent systems may soon become the standard of care for challenging wound cases, ushering in a new era of precision wound management.

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025