The field of regenerative medicine has witnessed remarkable advancements in recent years, with 3D-printed organ scaffolds emerging as a promising solution for tissue engineering. Among the critical factors influencing their success, pore optimization stands out as a pivotal element that determines the scaffold's functionality, cellular behavior, and eventual integration into the host tissue. Researchers are now delving deeper into the intricate balance between porosity, mechanical strength, and biological performance to unlock the full potential of these structures.
Understanding the Role of Porosity in 3D-Printed Scaffolds
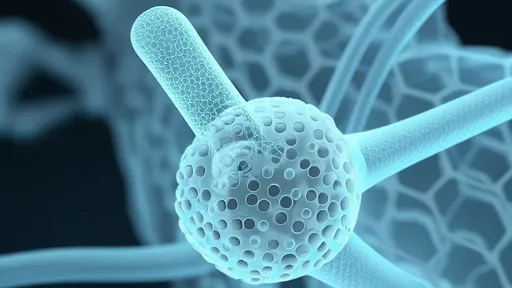
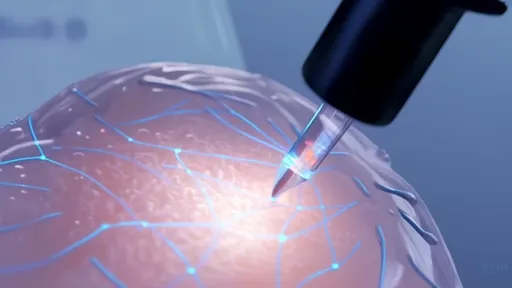
Porosity is not merely a physical characteristic of 3D-printed scaffolds; it is a dynamic feature that directly impacts cell migration, nutrient diffusion, and vascularization. A scaffold with inadequate porosity may hinder cell infiltration, leading to poor tissue regeneration, while excessive porosity could compromise its structural integrity. The challenge lies in designing a pore architecture that mimics the natural extracellular matrix, providing an optimal environment for cells to thrive. Recent studies have highlighted the importance of gradient porosity, where pore size varies across the scaffold to accommodate different cell types and mechanical demands.
Advanced computational modeling has become indispensable in this pursuit. By simulating fluid dynamics and stress distribution, researchers can predict how pores of varying shapes and sizes will behave under physiological conditions. For instance, hexagonal pore designs have shown superior nutrient flow compared to traditional square or circular pores, underscoring the need for geometry-specific optimization. These insights are paving the way for scaffolds that are not only biocompatible but also biomechanically robust.
Material Innovations and Their Impact on Pore Design
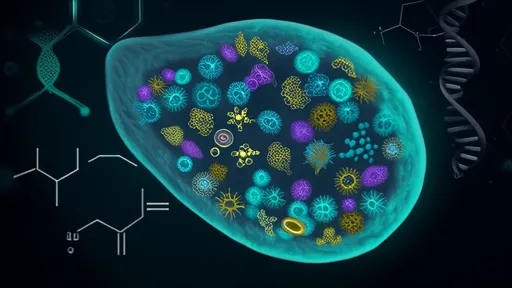
The choice of material plays a crucial role in determining the feasibility of pore optimization. Biopolymers like polycaprolactone (PCL) and gelatin methacryloyl (GelMA) are widely used due to their tunable properties. However, each material presents unique challenges. PCL, while mechanically stable, often requires post-processing to achieve desired porosity, whereas GelMA offers excellent cell adhesion but may lack the necessary stiffness for certain applications. To address these limitations, composite materials are gaining traction. For example, incorporating nanoparticles or hydrogels can enhance pore wall stability without sacrificing interconnectivity.
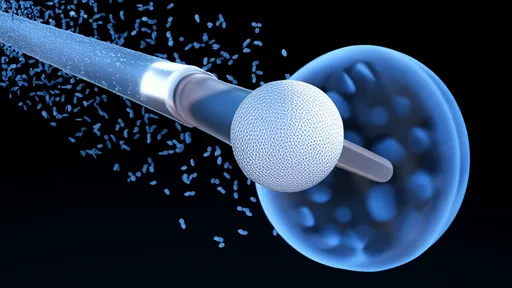
One groundbreaking approach involves the use of sacrificial materials during printing. By embedding water-soluble polymers or microspheres within the scaffold, researchers can create highly interconnected pores that dissolve after printing, leaving behind a meticulously designed porous network. This technique has proven particularly effective for creating vascular-like channels, which are essential for supplying oxygen and nutrients to cells in thicker scaffolds. The ability to precisely control pore size and distribution through such methods is revolutionizing the field.
Biological Implications of Optimized Porosity
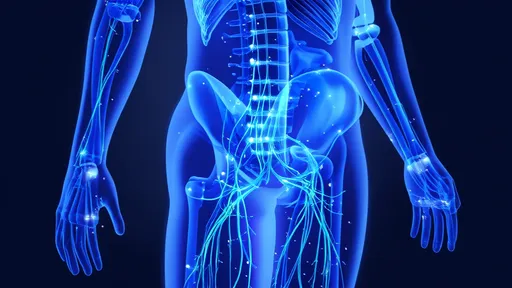
The ultimate goal of pore optimization is to foster an environment where cells can proliferate, differentiate, and form functional tissue. Studies have demonstrated that scaffolds with optimized porosity significantly enhance stem cell differentiation into target lineages, such as osteocytes or cardiomyocytes. This is attributed to the improved exchange of biochemical signals and mechanical cues within the porous network. Moreover, immune response—a critical factor in scaffold integration—is heavily influenced by pore size. Smaller pores tend to reduce inflammatory reactions, while larger pores promote macrophage polarization toward a regenerative phenotype.
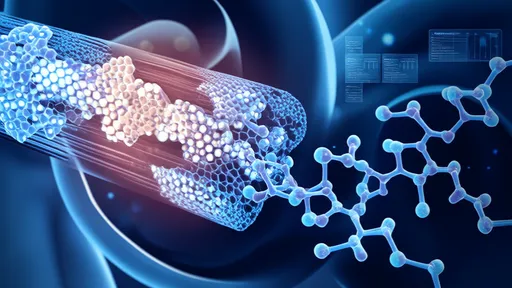
Another fascinating development is the incorporation of bioactive molecules within the pores. By embedding growth factors or drugs into the scaffold's porous structure, researchers can create localized delivery systems that guide tissue regeneration. For instance, vascular endothelial growth factor (VEGF) released from a scaffold's pores can accelerate blood vessel formation, addressing one of the major hurdles in engineering large tissues. These strategies highlight the multifaceted role of porosity in not just structural design but also biological functionality.
Challenges and Future Directions
Despite significant progress, several challenges remain in the quest for ideal pore optimization. One major hurdle is the scalability of fabrication techniques. While lab-scale 3D printers can produce scaffolds with exquisite pore detail, translating these methods to industrial-scale production without compromising precision is daunting. Additionally, the long-term degradation of scaffolds and its impact on pore structure—and consequently tissue regeneration—warrants further investigation. Researchers are exploring smart materials that degrade in sync with tissue growth, ensuring sustained mechanical support throughout the healing process.
The future of pore optimization lies in the convergence of multiple disciplines. Artificial intelligence, for instance, is being leveraged to analyze vast datasets on pore designs and their biological outcomes, enabling predictive modeling for customized scaffolds. Similarly, advancements in bioprinting technologies, such as multi-material extrusion, are opening new avenues for creating heterogeneous pore architectures tailored to complex organs like the liver or heart. As these innovations mature, the dream of fully functional 3D-printed organs may soon become a reality.
In conclusion, pore optimization in 3D-printed organ scaffolds represents a delicate interplay of engineering, biology, and material science. By continuing to refine pore design, researchers are not only enhancing the efficacy of these scaffolds but also inching closer to solving some of the most pressing challenges in regenerative medicine. The journey is complex, but the potential rewards—for patients and healthcare alike—are immeasurable.

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025