For decades, the placenta was considered a sterile environment, a protective barrier shielding the developing fetus from microbial invaders. This long-held belief shaped obstetric practices and our fundamental understanding of fetal development. However, groundbreaking research over the past fifteen years has radically transformed this perspective, revealing that the placenta harbors its own unique microbial ecosystem - findings that are reshaping reproductive medicine and neonatal care.
The Sterile Womb Paradigm Challenged
The concept of the "sterile womb" dominated medical thinking throughout most of the 20th century. Doctors and researchers believed that microbial colonization began during birth, as babies passed through the birth canal, or shortly after delivery. This paradigm began to crumble in 2010 when researchers at Baylor College of Medicine detected bacterial DNA in placental tissue. Their findings suggested that low-abundance microbial communities might exist in healthy pregnancies.
Subsequent studies using advanced sequencing technologies confirmed these initial observations. The placenta, it turns out, contains a sparse but metabolically active microbiome, with bacterial load estimates ranging from 50 to 500 times less dense than oral or gut microbiomes. This discovery opened an entirely new field of investigation into how these microbial communities might influence pregnancy outcomes and fetal development.
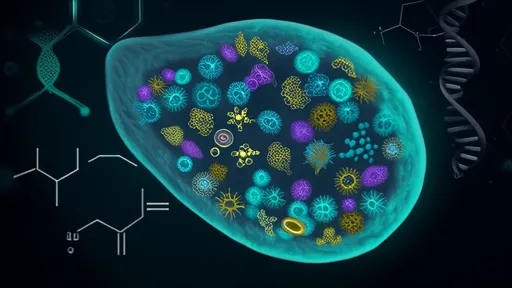
Characterizing the Placental Microbiome
Modern metagenomic sequencing has revealed that the placental microbiome predominantly consists of non-pathogenic commensal bacteria, with Proteobacteria, Firmicutes, Bacteroidetes, and Tenericutes being the most prevalent phyla. Interestingly, the placental microbial composition shows more similarity to the oral microbiome than to vaginal or intestinal microbiomes, supporting the "hematogenous spread" hypothesis - the idea that bacteria translocate from the mouth through the bloodstream to the placenta.
Research led by the University of Cambridge in 2021 identified distinct microbial signatures associated with different pregnancy complications. Preterm births showed higher abundance of Prevotella and Gardnerella species, while pregnancies complicated by preeclampsia demonstrated increased levels of Burkholderia. These findings suggest that microbial dysbiosis in the placenta may contribute to adverse pregnancy outcomes.
Maternal-Fetal Communication
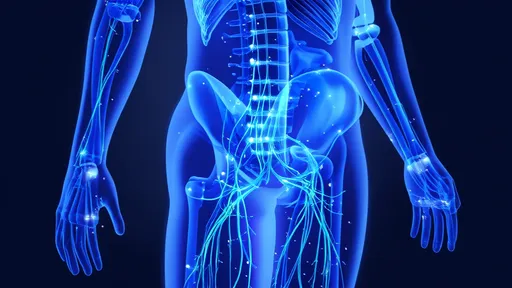
The placental microbiome appears to play a crucial role in immune system education and metabolic programming of the fetus. Studies using germ-free animal models demonstrate that the absence of microbial signals during gestation leads to profound immune dysfunction in offspring. Researchers at the University of Pennsylvania discovered that microbial metabolites from the placenta cross into fetal circulation, potentially influencing the development of the fetal immune system and metabolism.
Perhaps most remarkably, 2023 research published in Nature Medicine revealed that specific placental microbial metabolites can cross the blood-brain barrier and influence neurodevelopment. This finding provides a potential mechanistic link between maternal infections, microbiome alterations, and neurodevelopmental disorders like autism spectrum disorder and schizophrenia.
Clinical Implications and Future Directions
The emerging understanding of placental microbiology is transforming clinical practice. Obstetricians are reconsidering the routine use of broad-spectrum antibiotics during delivery, as these may disrupt the establishment of healthy neonatal microbiomes. Researchers are exploring microbiome-based diagnostics that could predict pregnancy complications weeks before clinical symptoms appear.
Several clinical trials are currently investigating targeted probiotic interventions during pregnancy to optimize placental microbial communities. Early results suggest that specific probiotic strains may reduce the risk of preterm birth and improve neonatal outcomes. However, experts caution that much more research is needed before microbiome modulation becomes standard practice in prenatal care.
As sequencing technologies become more sensitive and affordable, researchers anticipate discovering even more subtle interactions between placental microbes and fetal development. The next frontier involves understanding how these microbial communities vary across different populations and how environmental factors like diet, stress, and pollution influence placental microbiome composition.
The discovery of the placental microbiome represents one of the most significant paradigm shifts in reproductive biology in recent decades. As research continues to unravel the complex relationships between these microbial communities and pregnancy outcomes, we may be on the verge of a new era in prenatal medicine - one that recognizes the placenta not just as a physical barrier, but as a dynamic interface where microbial and human cells collaborate to shape the earliest stages of human life.

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025