The development of drug-eluting stents (DES) has revolutionized interventional cardiology by significantly reducing restenosis rates compared to bare-metal stents. However, the delayed endothelialization of these devices remains a critical challenge, as it can lead to late stent thrombosis and other complications. Recent advancements in stent coating technologies aim to accelerate endothelial recovery while maintaining antirestenotic properties, striking a delicate balance between healing and protection.
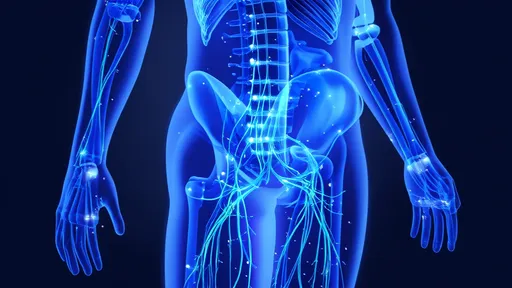
At the core of this innovation lies the concept of pro-healing coatings – surfaces engineered to actively recruit endothelial progenitor cells (EPCs) and promote their differentiation into functional endothelium. Unlike traditional DES coatings that primarily focus on drug delivery, these next-generation interfaces create a bioactive environment mimicking natural vascular biology. Researchers have explored various approaches, from peptide sequences that mimic extracellular matrix components to antibody-coated surfaces that capture circulating EPCs.
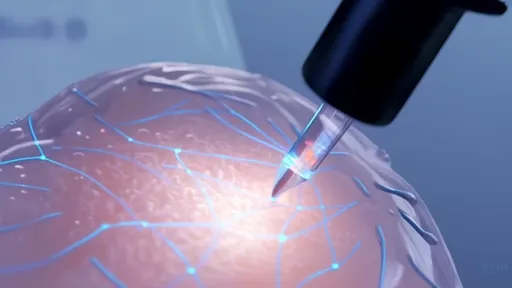
The CD34 antibody coating represents one of the most clinically advanced approaches in this field. By targeting the CD34 receptor present on endothelial progenitor cells, these coatings effectively "fish" for circulating repair cells and anchor them to the stent surface. Clinical studies have demonstrated faster endothelial coverage compared to conventional DES, with complete strut coverage observed as early as 28 days post-implantation. However, questions remain about the long-term functionality of these captured cells and their ability to form a truly protective endothelial layer.
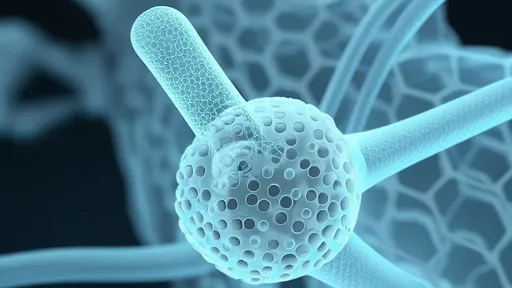
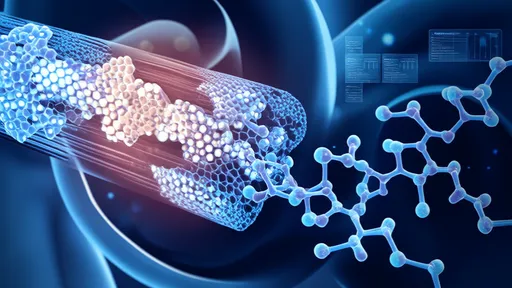
Another promising direction involves extracellular matrix (ECM)-mimetic peptides incorporated into stent coatings. These short amino acid sequences, such as the ubiquitous RGD motif, provide recognizable docking sites for endothelial cell adhesion while simultaneously promoting cell migration and proliferation. More sophisticated versions combine multiple bioactive peptides to recreate the complex signaling environment of natural blood vessels. Some experimental coatings even incorporate growth factors like VEGF in controlled-release systems to guide endothelial maturation.
The emergence of nitric oxide (NO)-releasing coatings has added another dimension to endothelialization strategies. NO serves as a crucial signaling molecule in vascular homeostasis, inhibiting platelet activation while promoting endothelial cell migration. Various NO donors have been integrated into polymer matrices, creating surfaces that not only resist thrombosis but also actively encourage endothelial cell recruitment. The challenge lies in achieving sustained NO release at physiologically relevant levels throughout the critical healing period.
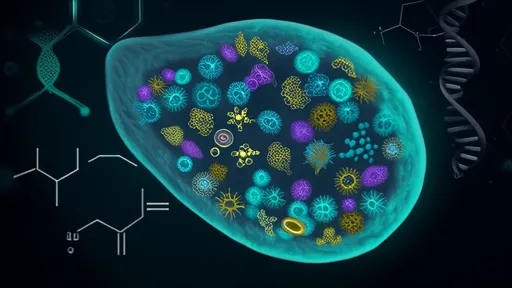
Biodegradable polymer platforms have gained particular attention as they address both the endothelialization delay and the long-term inflammatory risks associated with permanent polymer coatings. These temporary scaffolds provide initial drug delivery and surface bioactivity before gradually resorbing, leaving behind a clean metal surface that appears to endothelialize more readily. The degradation kinetics must be carefully tuned to match the vascular healing timeline – too rapid dissolution might compromise drug delivery, while overly prolonged presence could still interfere with healing.
Recent studies have highlighted the importance of topographical cues in stent coatings. Micro- and nano-scale surface patterns can significantly influence endothelial cell behavior, with certain textures promoting cell alignment and monolayer formation. Some experimental coatings combine these physical cues with biochemical signals, creating a synergistic effect that outperforms either approach alone. This biomimetic strategy recognizes that the native endothelium develops in response to both chemical and mechanical microenvironmental factors.
The clinical translation of these technologies faces several hurdles. While animal models provide valuable insights, differences in endothelialization rates between species complicate the extrapolation to human patients. Furthermore, the complex interplay between coating properties and patient-specific factors – such as diabetes or chronic kidney disease that impair endothelial function – requires careful consideration. Large-scale clinical trials will be essential to determine whether the improved endothelialization observed in preclinical studies translates into meaningful reductions in late adverse events.
Looking ahead, the field appears to be moving toward personalized stent coatings that could be tailored based on a patient's endothelial progenitor cell profile or genetic markers of healing capacity. Such approaches might combine diagnostic assessment with therapeutic intervention, optimizing outcomes for individual patients. Meanwhile, the integration of endothelialization-promoting coatings with bioresorbable vascular scaffolds represents another exciting frontier that could ultimately provide the ideal solution – temporary mechanical support with complete physiological restoration.
As research progresses, the ideal stent coating may not be one that simply delivers drugs or captures cells, but rather one that orchestrates the complex sequence of vascular healing – from initial platelet control to progenitor cell recruitment and finally to mature endothelium formation. This biological perspective represents a paradigm shift from the traditional engineering approach to stent design, recognizing that the most effective solutions will be those that work with the body's natural repair mechanisms rather than against them.

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025