The field of maternal and infant health has witnessed significant progress in recent years, particularly in the area of nutritional monitoring during lactation. As breastfeeding remains a critical phase for both mother and child, researchers have developed sophisticated dynamic monitoring technologies to ensure optimal nutrient intake. These innovations are transforming how healthcare providers support lactating women, moving beyond traditional static dietary assessments to real-time, personalized nutrition tracking.
Understanding the Challenges of Lactation Nutrition
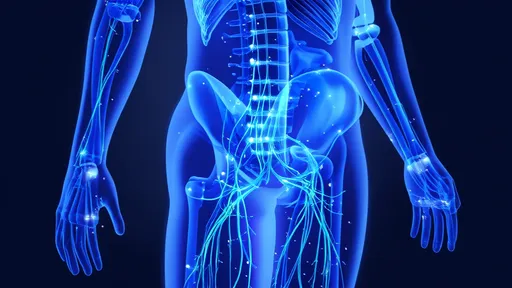
Lactation places extraordinary metabolic demands on mothers, requiring careful balancing of macronutrients, vitamins, and minerals. Conventional nutritional assessments often fail to capture the dynamic nature of breastfeeding, where a mother's nutritional needs can fluctuate significantly based on the infant's growth patterns, feeding frequency, and the mother's own physiological changes. This gap in monitoring has led to situations where deficiencies or excesses go undetected until clinical symptoms appear.
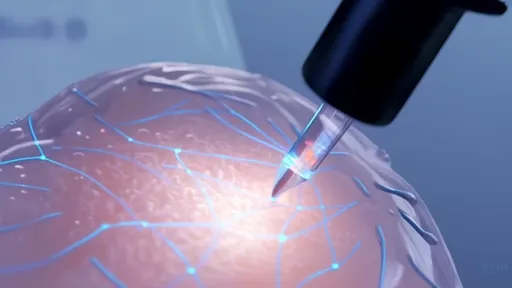
The development of dynamic monitoring systems addresses these limitations by incorporating multiple data streams. Wearable devices now track physiological markers like hydration levels, metabolic rate, and micronutrient status through non-invasive biosensors. These devices sync with mobile applications that analyze dietary intake, creating a comprehensive picture of the mother's nutritional status that updates throughout the day.
Technological Foundations of Modern Monitoring Systems
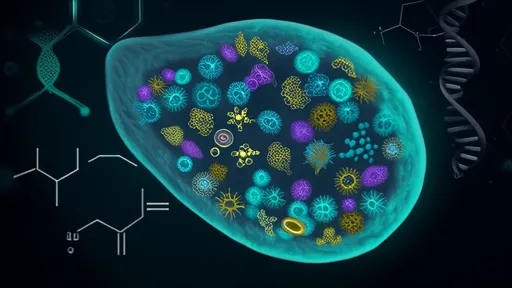
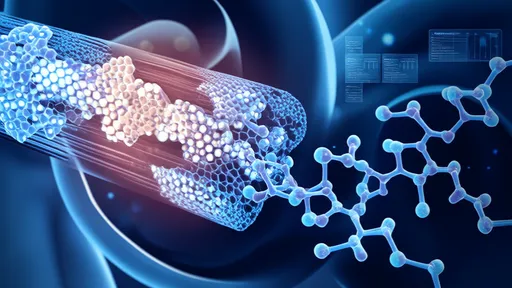
At the core of these advanced systems lie several groundbreaking technologies. Continuous glucose monitoring devices, originally developed for diabetes management, have been adapted to track energy metabolism in lactating women. New spectroscopic techniques allow for the measurement of key nutrients in breast milk through simple scanning devices. Artificial intelligence algorithms process this constant stream of data, identifying patterns and predicting potential nutritional gaps before they become problematic.
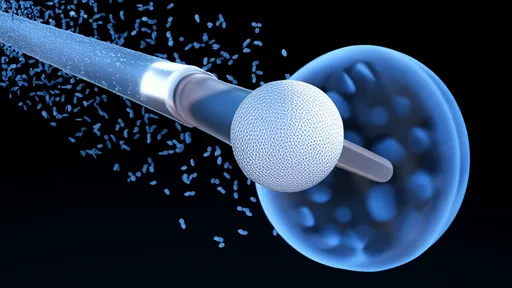
One particularly innovative approach involves the use of smart breast pumps equipped with nutrient sensors. These devices not only express milk but also analyze its composition in real time, providing immediate feedback about fat content, protein levels, and important micronutrients. This information helps mothers understand how their diet directly affects milk quality and allows for timely dietary adjustments.
Integration with Personalized Nutrition Platforms
The true power of dynamic monitoring emerges when combined with personalized nutrition platforms. These systems take the collected data and generate tailored dietary recommendations that evolve as the breastfeeding journey progresses. For instance, if the system detects declining levels of certain B vitamins, it might suggest specific food sources or supplementation strategies based on the mother's dietary preferences, allergies, and cultural food practices.
Some advanced platforms now incorporate genetic information to provide even more customized guidance. By analyzing genetic markers related to nutrient metabolism, these systems can predict how individual mothers might absorb or utilize particular nutrients during lactation. This level of personalization represents a significant leap forward from the one-size-fits-all nutritional advice that dominated the field for decades.
Clinical Applications and Health Outcomes
Early adoption of these technologies in clinical settings has shown promising results. Hospitals implementing dynamic monitoring for postpartum mothers report fewer cases of nutritional deficiencies and improved breastfeeding success rates. The ability to detect subtle changes in nutritional status allows for early intervention, preventing more serious complications for both mother and baby.
Perhaps most importantly, these technologies empower mothers with knowledge about their own bodies and their milk's nutritional profile. Rather than relying on generalized guidelines, women can make informed decisions based on their unique physiological data. This shift from passive recipient to active participant in nutritional management represents a fundamental change in postpartum care philosophy.
Future Directions and Challenges
As the technology continues to evolve, researchers are working to make these systems more accessible and user-friendly. Current challenges include reducing the size of monitoring devices, extending battery life, and improving the accuracy of non-invasive sensors. There's also ongoing work to integrate these systems with electronic health records, allowing seamless communication between mothers, nutritionists, and pediatricians.
The next generation of monitoring technology may incorporate environmental and lifestyle factors, such as stress levels and sleep patterns, which significantly impact lactation and nutrient metabolism. By creating a more holistic picture of maternal health, these systems could revolutionize not just nutritional monitoring but overall postpartum care.
While dynamic nutritional monitoring represents a significant advancement, experts emphasize that technology should complement rather than replace professional medical advice. The human element remains crucial in interpreting data and providing compassionate care during this vulnerable period. As these technologies become more widespread, maintaining this balance will be essential to their success in supporting breastfeeding mothers worldwide.

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025